Cultural Competence
in Healthcare Settings
Discussion Topics
Breakout Activity One:
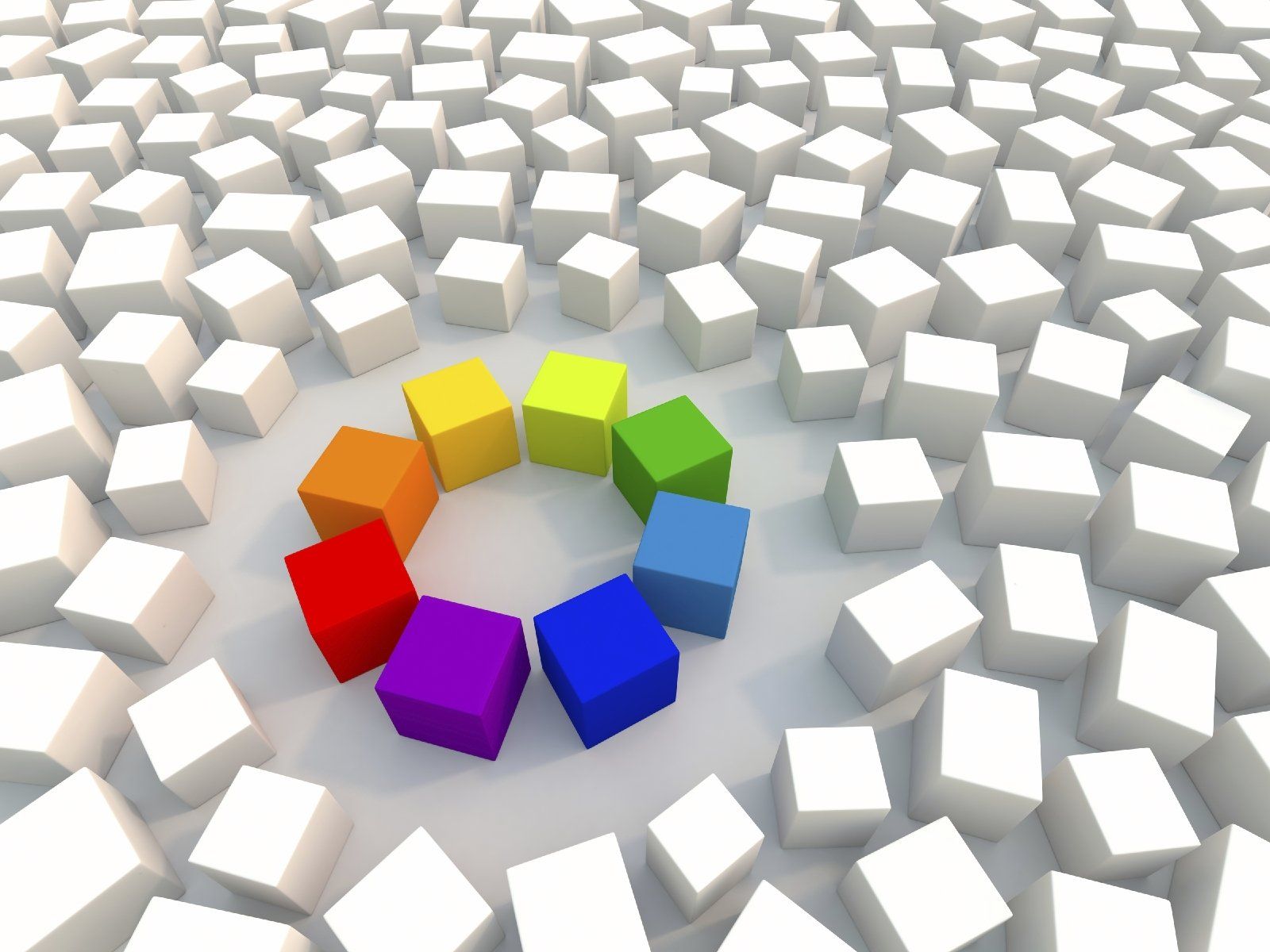
Cultural Competence Model
(from 'Blissfully Unaware' to 'Disrupters’)
Instructions:
In teams, self-assess where your team/ and the wider organisation sits in relation to EDI.
Your Leader will be the person born earliest in the year.
The Leader will guide you through the questions, ensuring all voices are heard.
Select a speaker to share a summary
when we return to the Main Room. If you prefer not to be the speaker, please nominate someone else.
Discuss
- Where are you today and why?
2. What barriers prevent you from moving up?
3. How does organisational culture play a role?
Consider: limited resources, traditional hierarchies, diverse staff. This graphic will be on the breakout webpage for reference.
Graphic is below to assist with this discussion.

Breakout Activity Two:
Private Paired Discussion - Psychological Safety
Creating a psychological safe environment allows people to be their true selves at work without the fear of bullying, harassment, isolation or judgement.
Discuss these questions with your partner:
- What is psychological safety in the workplace?
2. How can a psychologically safe environment support cultural competence?
3. What are the potential risks to workplace psychological safety?
4. How can Leaders identify and mitigate these risks?
Breakout Activity Three: Everyday Experiences
Instructions
In pairs/small teams, share examples of non-inclusive behaviours or language, that you or someone else may have experienced:
What was it?
What was the impact?
What would have changed the situation?


Breakout Activity Four: Case Studies
Instructions
Your
Leader will be the person born latest in the year.
The Leader will guide you through the questions, ensuring all voices are heard.
Discuss the Case Studies below and consider the related Discussion Prompts.
Next, consider the suggested Possible Allyship Responses.
Case Study 1: Misgendered Patient in a Ward
A nurse repeatedly refers to a patient, Alex, using the wrong pronouns, even after Alex has gently corrected them. Another staff member overhears and notices Alex becoming increasingly withdrawn.
Discussion Prompts:
- As a colleague, what should you do in the moment?
- How can you affirm Alex’s identity without escalating conflict?
- What longer-term steps could you take to promote inclusive practice on the ward?
Possible Allyship Responses:
Immediate Response: Politely correct the nurse by modelling the correct pronouns. Check in with Alex afterwards to validate their identity and wellbeing.
Private Follow-Up: Speak privately with the nurse to explain why pronoun use matters and share resources on inclusive practice.
Systemic Action: Encourage training on inclusive language and ensure ward policies highlight respect for gender identity.
Case Study 2: Cultural Food Needs Overlooked
Fatima, a patient recovering from surgery, is served meals that do not meet her religious dietary needs. When she asks staff if there are alternatives, a healthcare assistant dismisses her request, saying, 'It’s just food—you’ll be fine.’
Discussion Prompts:
- What could an ally do to support Fatima in this situation?
- How can you balance cultural sensitivity with organisational processes (menus, dietary policies, etc.)?
- What changes could be made systemically to prevent this from happening again?
Possible Allyship Responses:
Immediate Response: Acknowledge Fatima’s concern, apologise, and escalate to catering staff or a supervisor to find an appropriate meal option.
Private Follow-Up: Have a respectful conversation with the healthcare assistant about the impact of dismissing patient needs.
Systemic Action: Work with patient services to ensure culturally appropriate meals are available and staff are trained on dietary requirements.
Case Study 3: Racist Comment in the Staff Room
During a break, a doctor makes a disparaging remark about a patient’s accent, implying it makes them less credible. Some colleagues laugh, while others remain silent. A junior nurse feels uncomfortable but isn’t sure how to respond.
Discussion Prompts:
- What should an ally do in this situation?
- How can someone challenge bias while maintaining professionalism?
- What’s the impact if no one speaks up?
Possible Allyship Responses:
Immediate Response: Address the comment calmly, e.g. 'I don’t think that’s appropriate—accents don’t affect credibility.'
Private Follow-Up: Speak to the doctor later about how their remark could harm patient trust and team culture.
Systemic Action: Promote a zero-tolerance policy for discriminatory remarks and provide unconscious bias training.
Case Study 4: Interpreter Request Ignored
A patient who speaks little English requests an interpreter for a consultation. The doctor replies, 'It will take too long to arrange, let’s just get on with it,' and proceeds in English. The patient nods but looks anxious and confused.
Discussion Prompts:
- What should an ally do in the moment?
- How can you advocate for language access without undermining the clinician?
- What systemic changes could prevent this from happening again?
Possible Allyship Responses:
Immediate Response: Respectfully suggest that communication support is essential and offer to contact interpreter services.
Private Follow-Up: Speak with the doctor afterwards about patient safety and informed consent implications.
Systemic Action: Work with management to ensure easy access to interpreters and provide staff with training on language equity.
Case Study 5: Neurodivergent Colleague Overlooked
Jamie, a neurodivergent healthcare assistant, struggles with noisy environments and prefers written instructions. During handovers, a senior colleague rolls their eyes and says, 'We don’t have time to make special allowances for everyone.' Jamie goes quiet and stops asking clarifying questions.
Discussion Prompts:
- How can an ally support Jamie in the moment?
- What steps can be taken to promote inclusive communication in a fast-paced environment?
- How can you address the dismissive attitude of the senior colleague?
Possible Allyship Responses:
Immediate Response: Offer to provide Jamie with written notes or summaries and affirm that their needs are valid.
Private Follow-Up: Speak with the senior colleague about the importance of neurodiversity inclusion and respectful communication.
Systemic Action: Promote neurodiversity awareness training and embed adjustments into standard practice for handovers.
Case Study 6: Homophobic Joke in Theatre
While preparing for surgery, a consultant makes a joke about a gay celebrity, implying that gay men are 'dramatic' and 'unmanly.' Some theatre staff laugh, others stay silent, and one scrub nurse looks visibly uncomfortable.
Discussion Prompts:
- What could an ally do in this scenario?
- How can you challenge inappropriate humour in a high-pressure clinical setting?
- What difference does it make if senior staff model allyship?
Possible Allyship Responses:
Immediate Response: Respond calmly, e.g. 'Let’s keep the focus professional,' to signal the joke was inappropriate.
Private Follow-Up: Approach the consultant later to explain how their comment undermines inclusivity and professionalism.
Systemic Action:
Encourage leadership to model inclusive behaviour and integrate anti-discrimination policies into theatre culture.